- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
Disease Overview : Dilated Cardiomyopathy (DCM): When the Heart Muscles Become Enlarged and Weak — Know the Causes, Symptoms, and Treatment!
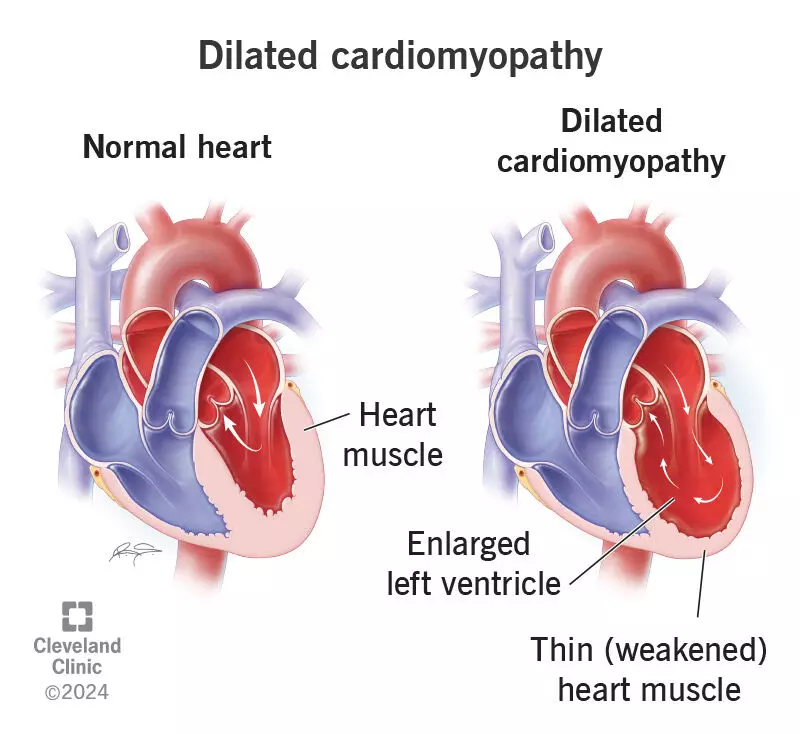
Dilated Cardiomyopathy (DCM) is a heart condition in which the heart muscles become weak and enlarged, reducing the heart’s ability to pump blood effectively. This affects blood flow to all parts of the body and gradually leads to symptoms resembling heart failure.
This disease can occur at any age — sometimes due to hereditary factors, and sometimes due to infections, alcohol use, certain medicines, or hormonal imbalance.
Early detection, regular check-ups, and following the treatment advised by the doctor are the keys to controlling this condition and improving the quality of life.
What is cardiomyopathy?
Dilated Cardiomyopathy (DCM) is a disease of the heart muscles. In this condition, the heart muscles become weak, stiff, or thick, causing the main pumping chamber of the heart (usually the left ventricle) to enlarge and lose its pumping strength. As a result, the body does not receive enough blood and oxygen, and symptoms similar to heart failure begin to appear.
What are the causes of cardiomyopathy?
Cardiomyopathy (DCM) can develop due to many reasons—sometimes the cause is not known (Idiopathic). It is not just a heart disease but a complex disorder linked to several body conditions and lifestyle factors. The main causes are as follows:
• Coronary artery disease (blockage in the heart vessels)
• High blood pressure
• Infection/Myocarditis: Heart muscle becomes inflamed after a viral infection
• Certain cancer medicines and other heart-damaging drugs/toxins
• Thyroid disorders, diabetes/metabolic syndrome, nutritional deficiencies (thiamine, selenium, L-carnitine)
• Excessive alcohol consumption, and some illegal drugs (cocaine, methamphetamine)
• Rarely, during the last months of pregnancy or a few months after delivery (Peripartum cardiomyopathy)
• Obstructive Sleep Apnea, sarcoidosis, hemochromatosis, etc.
• Persistent fast heartbeat (Tachycardia-induced), stress-related
• If anyone in the family has had cardiomyopathy or heart disease at a young age, inform your doctor — some forms are hereditary.
What are the common symptoms?
The symptoms of cardiomyopathy often appear gradually, and many people mistake them for normal tiredness or the effects of aging. However, these signs may indicate weakening of the heart (heart failure). The main symptoms are:
• Shortness of breath — first during exertion, then with minimal activity, and in severe cases even at rest
• Fatigue and weakness, reduced stamina for daily activities
• Swelling in the feet and legs, abdominal bloating, rapid weight gain (due to fluid retention)
• Breathing difficulty when lying down, waking up at night with breathlessness or coughing
• Fast or irregular heartbeat (palpitations), fainting or dizziness
• Chest pain
• Loss of appetite, feeling full quickly
When to consider it an emergency? Who is at higher risk?
If you experience chest pressure/pain, severe shortness of breath, fainting, or a sudden rapid heartbeat, go to the nearest emergency room (ER) immediately or call an ambulance.
Cardiomyopathy can occur at any age, but some people have a higher risk.
- If a family member has had Dilated Cardiomyopathy (DCM) or if someone in the family died suddenly at a young age due to cardiac arrest, the chances of other relatives developing this condition increase.
- This condition is seen slightly more often in men, although women can also be affected.
- Additionally, high blood pressure, diabetes, obesity, and smoking or alcohol consumption are major risk factors for cardiomyopathy.
Regular heart check-ups and adopting a healthy lifestyle are the best ways to reduce the risk of this disease.
How is it diagnosed?
Relying only on symptoms is not enough to detect cardiomyopathy — a proper diagnosis requires a thorough medical evaluation and modern tests to accurately assess heart function. The following methods are most important for diagnosing this condition:
• Doctor’s evaluation: symptoms, family history, medicine/alcohol history, and physical examination
• ECG, X-ray, and blood tests (such as hormones, kidney function, iron levels, BNP, etc.)
• Echocardiography (2-D Echo Doppler): helps detect heart enlargement and pumping capacity (LVEF)
• Holter monitor, cardiac MRI, and coronary tests (to rule out CAD), as needed
• Genetic counseling/testing in certain cases
What is the treatment?
The treatment of cardiomyopathy depends on the patient’s condition and the underlying cause. Starting treatment at the right time can improve heart function and prevent complications. The main treatment options are as follows:
• Medicines to control high blood pressure, if present
• Heart-specific medicines prescribed and adjusted by the doctor from time to time
• If there is heart failure, some patients may require a small device like a pacemaker (sometimes a special device), which needs to be implanted through surgery
• In severe cases, a heart transplant may be considered — this decision is made by the cardiology team after evaluating your condition
What daily precautions are needed?
For patients with cardiomyopathy, not only medicines but also daily habits make a significant difference.
By following a healthy diet, regular monitoring, and a balanced lifestyle, the heart can be kept stronger and worsening of the condition can be prevented. The essential precautions are:
• Control salt intake: as advised by the doctor (~1.5–3 grams/day; follow individual guidance)
• Daily weight monitoring: if there is a sudden increase of 1–2 kg, contact your doctor/clinic
• Stop smoking and alcohol; strictly avoid any narcotic substances
• Exercise: regular, moderate-intensity exercise as guided by the doctor; avoid excessive or competitive sports
• Vaccinations: flu and pneumococcal vaccines (ask your doctor)
• Take medicines on time; do not take NSAIDs and other heart-harming drugs without medical advice
• Nutrition: adequate protein, fresh fruits and vegetables; if overweight, reduce weight safely
• If you have snoring or asthma-like symptoms during sleep, get checked for sleep apnea
Why is family screening important?
If there is a history of DCM or sudden death at a young age in the family, it is useful for first-degree relatives (parents, siblings, children) to undergo ECG/Echo periodically (usually every 3–5 years).
Many cases are genetic — therefore, genetic counseling is helpful.
What are the possible serious outcomes?
If cardiomyopathy is not treated in time or if medicines are not taken properly, it can lead to several serious complications. These problems can sometimes be life-threatening. The major possible complications are:
• Sudden cardiac arrest / dangerous arrhythmias
• Atrial fibrillation (irregular heartbeat)
• Blood clots — stroke / clot in the lungs
• Worsening of heart failure
What is the prognosis and what are the future possibilities?
The prognosis of cardiomyopathy depends on how severe the weakness of the heart is and how well the patient adheres to treatment and lifestyle changes. Although this disease may not be completely curable, it can be controlled with timely treatment and continuous care.
The good news is that in many patients, when treatment is started on time and medicines are taken regularly, the size of the heart and its pumping capacity (Ejection Fraction) can gradually improve. This enhances the quality of life, reduces symptoms like fatigue and shortness of breath, and allows patients to return to their normal daily routine.
However, it is important to remember that stopping medicines suddenly or making changes without the doctor’s advice can cause the disease to worsen again. Therefore, regular follow-up, review of medications, and maintaining a healthy lifestyle are extremely important.
A balanced diet, reduced salt intake, stress management, and periodic check-ups together can help a cardiomyopathy patient live a long and active life.
What should you ask your doctor?
Awareness and understanding by the patient are extremely important in the treatment of cardiomyopathy.
Asking your doctor open and clear questions not only helps you understand the disease better but also makes it easier to follow the right treatment and lifestyle. During your conversation with the doctor, be sure to ask the following questions:
What is the likely cause of my cardiomyopathy?
Knowing the cause can help prevent the recurrence of this disease in the future, and other family members can also remain alert.
If this happened due to another condition, will treating that condition improve my symptoms?
Sometimes conditions like thyroid disorder, diabetes, or infections, when controlled, can improve heart function.
What is the most appropriate treatment for me — medicines or a surgery/device?
The doctor will determine whether you only need medicines or whether you may benefit from special devices such as a pacemaker or ICD based on your condition.
What lifestyle changes do I need to make?
Ask for specific guidance regarding diet, salt intake, exercise, stress management, and sleep patterns.
Am I at risk of heart failure?
This is important to know so that you can get regular check-ups and keep an eye on any symptoms.
Might I need a heart transplant in the future?
This question is especially relevant in advanced stages of the disease. The doctor will inform you under what circumstances this option may be considered.
Timely Detection and Careful Management for Heart Protection
Early detection of Dilated Cardiomyopathy, guideline-based medical treatment, ICD/CRT devices in selected patients, and lifestyle modifications — all of these together can reduce hospitalizations, complications, and the risk of death.
Family screening and regular follow-up are equally important.
Heidenreich PA et al: 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 3;79(17):e263-421, 2022
McDonagh TA et al: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 42(36):3599-726, 2021
Arbelo E et al: 2023 ESC Guidelines for the management of cardiomyopathies. Eur Heart J. 44(37):3503-626, 2023
Bozkurt B et al: Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 134(23):e579-646, 2016
Dr Prem Aggarwal, (MD Medicine, DNB Cardiology) is a Cardiologist by profession and also the Co-founder of Medical Dialogues. He is the Chairman of Sanjeevan Hospital in Central Delhi and also serving as the member of Delhi Medical Council

