- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
“Ventricular Septal Defect – Know Everything!”
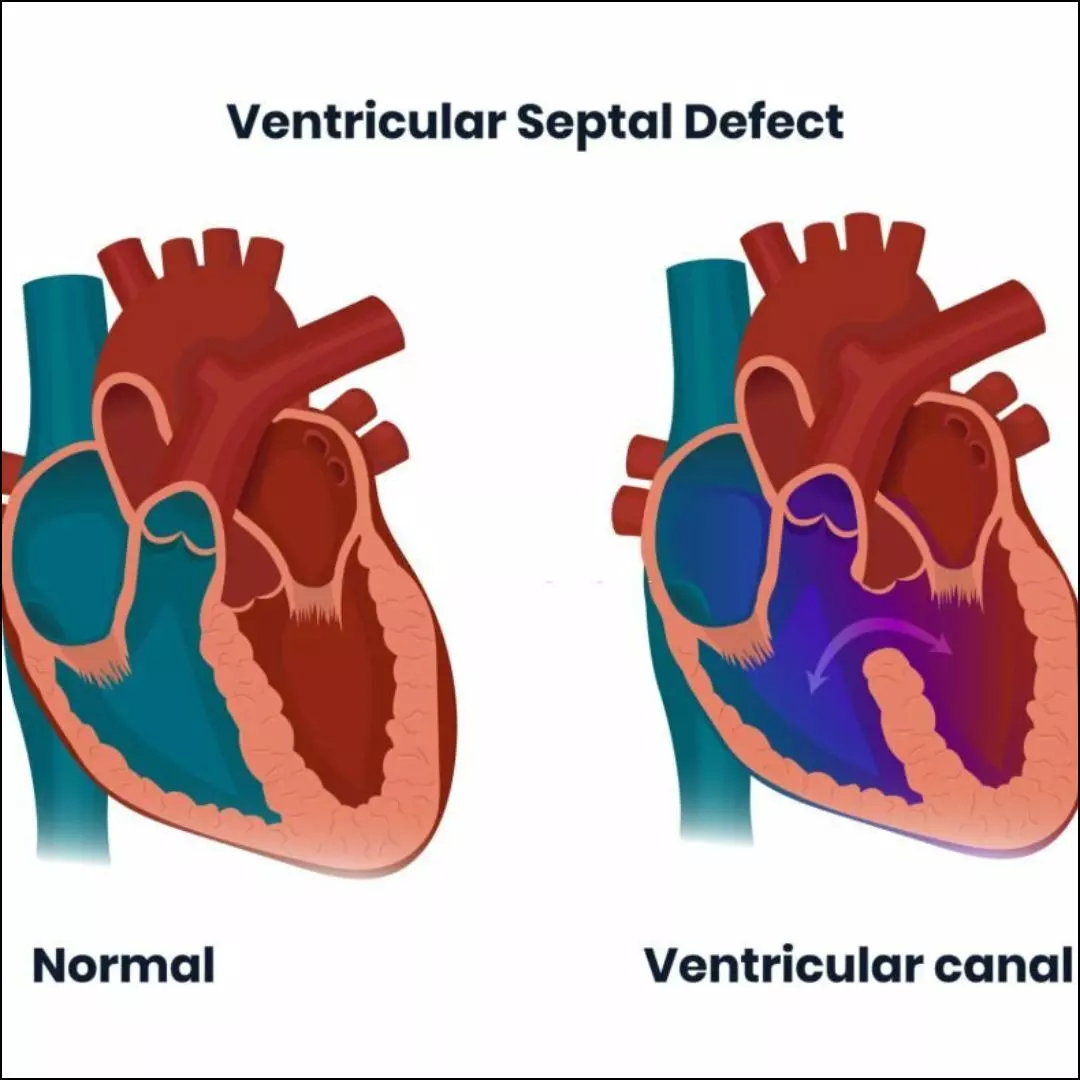
Ventricular Septal Defect (VSD) is the most common congenital heart disease found in children. In this condition, a hole develops in the wall separating the two lower chambers of the heart, but many parents are not fully aware of what it means.
Small VSDs may close on their own, while larger defects require treatment. What exactly is this condition, why does it occur, and when does it become dangerous? Let’s understand it.
What is a Ventricular Septal Defect?
Our heart has four chambers — two upper chambers (atria) and two lower chambers (ventricles). The two lower ventricles are separated by a thin wall called the interventricular septum. If a hole develops in this wall, it is called a Ventricular Septal Defect (VSD).
It is the most common congenital heart disease seen in children. When this hole is present, the oxygen-rich blood from the left ventricle flows into the right ventricle. This causes excess blood to reach the lungs, which can lead to problems over time.
Around 30% of all congenital heart disease cases worldwide are due to VSD. Most small VSDs do not cause major problems and often close on their own with time.
Types of Ventricular Septal Defect — What does each type of hole mean?
A ventricular septal defect is not the same in every child. The location and size of the hole determine the severity of the condition, the symptoms, and the treatment required.
1. Perimembranous Ventricular Septal Defect: This occurs in the thin upper membranous part of the ventricular septum. It is the most common type — about 70–80% of all VSDs fall into this category.
2. Muscular Ventricular Septal Defect: This occurs in the lower muscular portion of the heart wall. There may be one large hole or several small holes. The good thing is that these holes often become smaller or close on their own as the child grows. Such children usually only need regular follow-up with a doctor.
3. Inlet Ventricular Septal Defect: This type occurs near the atrioventricular (AV) valves. It is often seen along with larger congenital defects (such as AV canal defect). Treatment for such cases is typically done in specialized centers.
4. Supracristal / Outlet Ventricular Septal Defect: This is located just below the pulmonary valve, near the pathway that carries blood toward the lungs. This type is more commonly found in India, China, and Japan. It carries a risk of damaging the aortic valve over time, which is why doctors often advise surgery even for relatively small holes.
If a ventricular septal defect has been detected in your child, do not panic.
Just consult a specialist pediatric cardiologist to understand what type of hole it is, how big it is, and whether treatment is needed.
What are the causes of Ventricular Septal Defect?
In most children, the exact cause of VSD is not known. However, several factors are believed to be associated with it:
● The heart not forming completely during fetal development
● Genetic and environmental factors
● Certain genetic conditions such as Down syndrome
● Infections during pregnancy (such as rubella)
● Effects of alcohol, smoking, or certain medications during pregnancy
● If either parent had a ventricular septal defect in childhood, the risk is higher in the baby
Symptoms of Ventricular Septal Defect – What signs may appear at different ages?
The symptoms of a ventricular septal defect depend on the size of the hole.
(1) In Infants
- Small Ventricular Septal Defect:
Infants with a small ventricular septal defect usually do not show any noticeable symptoms. The baby feeds normally, plays well, and gains weight appropriately. This condition is often detected only when the doctor hears a murmur (a blowing sound) during a routine examination.
- Moderate or Large Ventricular Septal Defect:
In infants with a moderate or large ventricular septal defect, symptoms begin to appear a few weeks to a few months after birth. Such babies may get tired quickly while feeding and may pause frequently to catch their breath. Rapid breathing or mild shortness of breath (tachypnea) may also be seen. They may sweat during feeding or even while crying.
These infants do not gain weight at the expected rate, making the body look thin or weak. Frequent chest infections, coughing, or wheezing are also common. Due to increasing discomfort, the baby may become irritable, and sleep may also be disturbed.
(2) In older children and adults
In some cases, a small ventricular septal defect goes undetected in childhood and is diagnosed later in life. Such children or adults generally do not have major problems and lead a normal life.
Sometimes, a mild murmur heard during a routine health checkup leads to detection. Occasional mild fatigue may be present, but most such individuals remain active and do not require any special restrictions.
How do doctors diagnose a Ventricular Septal Defect?
Doctors diagnose a ventricular septal defect by assessing the structure and functioning of the heart through various methods.
1. Physical Examination:
Firstly, the doctor listens to the heart sounds with a stethoscope.
In small ventricular septal defects, a loud holosystolic murmur—a blowing sound heard throughout systole—is often heard, and sometimes a slight vibration (thrill) can also be felt on the chest.
In contrast, in large ventricular septal defects, the murmur may be relatively softer and of a “blowing” type. Along with this, if the defect is large, the child may show signs of heart failure such as rapid breathing, fast heartbeat, poor weight gain, or an enlarged liver felt in the upper abdomen.
2. Echocardiography (ECHO):
Echocardiography is the most important and reliable test for diagnosing a ventricular septal defect.
This test clearly shows the internal structure of the heart, the location, size, and type of the ventricular septal defect, the amount of blood flowing through the hole, and the pressure on the lungs. Because of this, diagnosis through echocardiography is almost 100% accurate, and the treatment plan is based directly on the findings of this report.
3. Other supportive tests:
● ECG (Electrocardiogram): This test gives an idea of the pressure on the heart chambers and any enlargement. In large ventricular septal defects, increased load on the left or right side of the heart may be seen on the ECG.
● Chest X-ray: This shows the size of the heart and the amount of blood in the lungs. In large ventricular septal defects, the heart may appear enlarged and the lung blood vessels may look more prominent.
● Other advanced tests: In some complex or rare cases, doctors may perform MRI or cardiac catheterization, which provide a detailed assessment of heart structure, pressures, and the exact amount of shunt.
What is the goal of treatment?
While planning the treatment of a ventricular septal defect, doctors firstly consider which important health goals need to be achieved so that the child’s growth remains safe and no serious problems arise in the future.
● To control symptoms of heart failure in infants (such as fast breathing, poor weight gain, and recurrent infections)
● To protect the heart valves, lungs, and heart muscle from long-term damage.
● To prevent severe complications such as persistent high pressure in the lungs and Eisenmenger syndrome
● To help the child achieve normal growth and live a normal, healthy life
How is a ventricular septal defect treated?
The treatment of a ventricular septal defect can be different for every child because it depends on how large the hole is, how much pressure it is putting on the heart, and how many symptoms the child is showing.
1. Small Ventricular Septal Defect
Most small ventricular septal defects close on their own by the age of 2–4 years. Children with a small ventricular septal defect generally do not need any special medicines or surgery.
In such cases, doctors only perform regular checkups to monitor whether the hole is gradually becoming smaller. There are no restrictions on the child’s daily activities, and most children can live a completely normal life.
2. Moderate or Large Ventricular Septal Defect
When the ventricular septal defect is large, or when the child shows symptoms such as rapid breathing, sweating, or poor weight gain, doctors may start some medications. These may include medicines that improve the heart’s function, medicines that lower blood pressure, and medicines that remove excess fluid from the body to reduce the load on the heart.
These medicines only reduce symptoms; they do not close the ventricular septal defect. If symptoms persist despite medications, or if the VSD does not become smaller on its own, then surgery is planned.
3. Surgery (Open Heart Surgery) – Permanent and Safe Treatment
Children with moderate and large ventricular septal defects often require surgery. Most specialists recommend performing this surgery before the child is 1 year old so that the heart and lungs do not suffer permanent damage. In certain special situations such as late diagnosis or mild symptoms — surgery may be done during adolescence.
With modern techniques, VSD surgery is considered very safe and highly successful; most children are completely cured with this treatment.
4. Transcatheter Device Closure
In certain specific situations, especially in children with muscular ventricular septal defects, the defect can be closed without open-heart surgery.
In this technique, a small device is delivered to the heart through a thin tube (catheter), and the device is positioned over the hole to close it. This method is suitable only for children whose heart anatomy allows this procedure. Currently, it is available only in a few specialized centers.
5. Pulmonary Artery Banding
In some severe situations — such as very small or weak infants, or children who have multiple ventricular septal defects — immediate complete surgery may not be possible.
In such cases, doctors firstly place a band around the pulmonary artery to control the blood flow going to the lungs and prevent lung damage. When the child becomes older and stronger, the second stage involves complete repair of the ventricular septal defect and removal of the pulmonary artery band.
What can happen, if a ventricular septal defect is not treated at the right time?
Leaving a large ventricular septal defect untreated for a long time can lead to several complications:
1. Infective Endocarditis:
In children with a ventricular septal defect, the risk of bacteria sticking to the inner lining of the heart increases—often due to poor dental hygiene or bacteria from the mouth entering the bloodstream. If not treated in time, it can cause permanent damage to the heart.
2. Aortic Regurgitation:
Some types of ventricular septal defects especially supracristal and perimembranous, pull the aortic valve toward the hole. This causes the valve to leak, increasing the load on the left ventricle. Over time, this can weaken the heart and may require surgery.
3. Subaortic Stenosis or Double-Chambered Right Ventricle:
The high-velocity jet of blood flowing through the hole can cause unwanted tissue to form inside the heart, creating a new obstruction. This can lead to breathlessness, fatigue, and increased pressure on the heart. Such children often require surgery later on.
4. Eisenmenger Syndrome – The Most Serious Complication:
If a large ventricular septal defect is not treated on time, permanent high pressure develops in the lungs. Eventually, the direction of blood flow reverses (right-to-left shunt), causing blue-colored blood to circulate in the body called Cyanosis. In this condition, difficulty in breathing, thickening of blood, and damage to the heart and other organs are common. At this stage, surgery for VSD becomes almost impossible.
What is the prognosis for the patient?
The patient's long-term outcome with a ventricular septal defect depends largely on the size of the hole, the age at which it is detected, and whether timely treatment is provided. The good news is that with modern medical care, the long-term prognosis for most children is excellent.
● Small Ventricular Septal Defect:
Children with a small ventricular septal defect almost always have an excellent prognosis. About 30–50% of small VSDs close on their own by the age of two, and by the age of four, most become so small that they have no practical impact. Such children grow normally and lead a completely normal life.
● Moderate Ventricular Septal Defect:
Moderate-sized ventricular septal defects can behave in different ways—some become smaller on their own, in some children the symptoms can be managed fully with medications, while others may require surgery.
However, with timely diagnosis, regular monitoring, and appropriate decision-making, these children also have a good prognosis and can lead healthy, normal lives.
● Large Ventricular Septal Defect:
Large ventricular septal defects usually do not close on their own and may cause recurrent infections, poor weight gain, or signs of heart failure in children. In such cases, surgery is often decisive and life-saving. After surgery, children catch up well in growth. If surgery is done at the right time, life expectancy is nearly normal.
What problems can occur after surgery?
Ventricular septal defect surgery is generally very safe, and most children recover without any major problems. However, some children may experience a few mild issues:
1. Right Bundle Branch Block:
This is a type of change that appears on the ECG. In most children, it does not cause any difficulty, and they remain completely normal.
2. Complete Heart Block:
In very rare cases, the heart’s electrical signals may get affected. In such situations, a pacemaker may be required.
3. Mild Leakage of Some Valves:
There may be slight leakage in the tricuspid or pulmonary valve. In most cases, this is very minor and does not cause any discomfort to the child.
4. Mild Learning or Attention Difficulties:
A small number of children may experience mild issues related to learning or concentration later in life. The good thing is that most children can attend school normally and lead an everyday life without significant challenges.
How should the patient be cared for at home?
After a ventricular septal defect is diagnosed or treated, proper home care plays a very important role in keeping the child healthy and preventing complications. Parents should follow these essential guidelines:
● Medication-related precautions:
Give all medicines to the child exactly as prescribed by the doctor. If antibiotics have been given, completing the full course is extremely important. Do not give aspirin to the child without the doctor’s advice, as it can be harmful.
● Dental care:
Good dental hygiene is very important for children with a ventricular septal defect, because bacteria from the teeth and gums can enter the bloodstream and affect the heart. Teach the child to brush and floss regularly. Some children may require antibiotics before dental cleaning or dental procedures—always check with your doctor regarding this.
● Other important advice:
If the child is not gaining weight properly, consult the doctor or a dietitian about high-calorie supplements. Avoid any type of body piercing, as this can allow bacteria to enter the bloodstream. Ensure that all follow-up visits are done on time, and if the doctor advises, have the child evaluated by a pediatric cardiologist regularly.
When to consult a doctor?
If your child shows unusual fatigue during daily activities or struggles to breathe, these may be symptoms related to a ventricular septal defect. If you notice such signs, contact a pediatrician or a pediatric cardiologist immediately.
● Rapid breathing
● Sweating while feeding or getting tired quickly during feeding
● Frequent chest infections
● Not gaining weight or weight stagnation
● Skin, lips, or nails turning blue (cyanosis)
Seek medical attention immediately if:
• A baby younger than 3 months has a fever of 100.4°F (38°C) or higher
• A baby older than 3 months has a fever of 102.2°F (39°C) or higher
• The child has difficulty breathing
• The skin, lips, or nails appear blue or very pale
If a doctor is not available, do not wait — go immediately to the nearest emergency or urgent care center.
Why is regular monitoring necessary?
Regular monitoring helps ensure that the heart continues to function well, the defect is healing as expected, and no new complications are developing.
1. Small–moderate ventricular septal defects that do not require surgery:
Such children require periodic clinical examinations and ECHOs to check whether the hole is becoming smaller on its own and to ensure that there is no new effect on the heart valves or the lungs.
2. Children who have undergone ventricular septal defect surgery:
After surgery, regular follow-up with a cardiologist is necessary for the first few years. If there is no residual defect, no high pressure in the lungs, and no valve-related problems, the child can go on to live a normal and healthy life.
3. Children with Down syndrome:
These children have a higher risk of congenital heart defects from birth, so routine ECHO examinations are especially important.
Timely monitoring is the key to safety
Regular monitoring and timely evaluations ensure that the child remains safe from any complications related to a ventricular septal defect and is able to live a healthy, normal life.
Minette MS et al: Ventricular septal defects. Circulation. 114(20):2190-7, 2006
Anderson B: Introduction to congenital heart disease. In: Anderson B, ed: A Sonographer's Guide to the Assessment of Heart Disease. MGA Graphics; 2013
Bernier PL et al: The challenge of congenital heart disease worldwide: epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 13(1):26-34, 2010
Graham TP Jr et al: Ventricular septal defect and aortic regurgitation. Prog Pediatr Cardiol. 14(2):163-73, 2001
Dr Prem Aggarwal, (MD Medicine, DNB Cardiology) is a Cardiologist by profession and also the Co-founder of Medical Dialogues. He is the Chairman of Sanjeevan Hospital in Central Delhi and also serving as the member of Delhi Medical Council

