- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
Aortic Valve Stenosis (AVS) When the main heart valve becomes narrow — know the symptoms and treatment of this serious heart condition
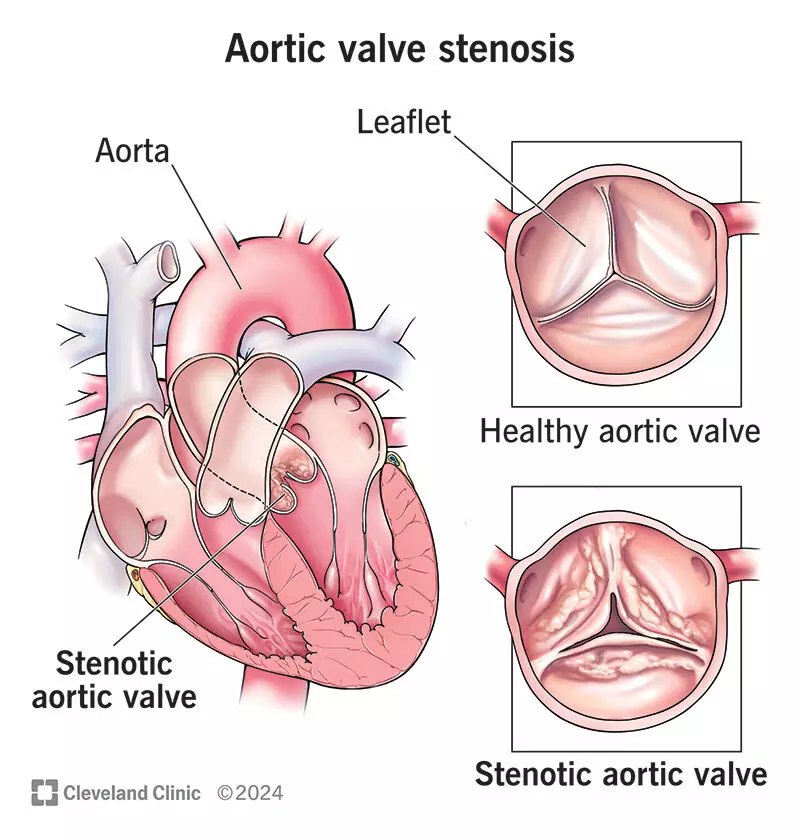
In aortic valve stenosis, the main valve of the heart — called the aortic valve — gradually becomes narrow and stiff. This valve controls the blood flow between the left ventricle of the heart and the aorta.
When this valve becomes tight, the flow of blood from the left ventricle to the rest of the body becomes restricted, forcing the heart to work harder to pump blood throughout the body. Over time, this extra pressure weakens the heart muscle and can lead to a condition like heart failure.
This disease usually progresses slowly — symptoms may not appear for 10 to 15 years. But once it becomes severe, dangerous symptoms such as shortness of breath, chest pain, and fainting can appear.
Timely diagnosis and proper treatment, especially valve replacement, can save a life.
What are the main causes of Aortic Valve Stenosis?
Aortic valve stenosis can occur due to several reasons — some are age-related, while others are congenital or develop because of other illnesses.
- Calcium buildup with aging: As calcium deposits accumulate on the valve leaflets, they become stiff and narrow. This is the most common cause.
- Congenital defect (Bicuspid Valve): Normally, the valve has three leaflets, but some people are born with a two-leaflet (bicuspid) valve.
- Rheumatic fever: Infection during childhood or adolescence can damage the valve.
- Genetic factors: The risk increases if this disease runs in the family; bicuspid valves are more commonly seen in males.
- Comorbidities: High blood pressure, high cholesterol, diabetes, and kidney diseases can accelerate the progression of the disorder.
- Effects of radiation therapy: Radiation treatment to the chest can damage the valve.
Symptoms — When to be alert?
Often, no symptoms appear for a long time; mild or moderate stenosis may take 10–15 years to become severe. When it becomes serious, the following symptoms may appear:
- Shortness of breath – especially while walking or climbing stairs.
- Unusual fatigue or weakness.
- Pain or tightness in the chest, neck, or arms (angina).
- Heartbeats feeling fast or irregular (palpitations).
- Dizziness or fainting – especially after exertion or stress.
- Shortness of breath when lying down, or sudden breathlessness at night.
- Swelling in the legs or ankles.
Visit the hospital immediately if: breathing becomes rapidly worse, there is severe chest pain, fainting occurs, the lips turn blue, or the condition suddenly deteriorates.
Who is at higher risk?
Some individuals have a greater likelihood of developing aortic valve stenosis
- Age 65 years or older.
- Having a congenital bicuspid aortic valve.
How is it diagnosed?
Accurate diagnosis of Aortic valve stenosis is very important, because its symptoms can often resemble those of other heart diseases. Doctors use various tests to determine how narrow the valve has become, how much pressure the heart is under, and when treatment is needed. Let us understand this process in detail:
1. Physical Examination: The doctor listens for a systolic murmur with a stethoscope. This is a special type of “whooshing” sound heard in the upper right part of the chest, sometimes radiating to the neck. This murmur can be the first sign that the valve is becoming narrow.
2. Echocardiogram — the most important test : This test uses ultrasound waves to create a real-time image of the heart’s structure, valve movement, and the flow of blood. Several key measurements are taken during this test:
Maximum blood flow velocity (Maximum Velocity): This shows how fast blood is flowing through the narrowed valve. Higher velocity indicates more severe narrowing.
Mean Pressure Gradient: This measures how much resistance blood faces while passing through the valve. As the valve becomes more narrow, the pressure gradient increases. A high gradient indicates severe stenosis.
Valve Area: This shows the actual size of the valve opening. If the valve area is 1.0 cm² or less, it is considered severe aortic valve stenosis.
Echocardiography not only confirms the diagnosis but also shows how far the disease has progressed.
3. Additional supportive tests : Sometimes, to clarify the condition or in complex cases, other tests are also performed:
ECG: Shows the electrical activity of the heart and any rhythm abnormalities.
Chest X-ray: Shows the size of the heart, lung congestion, or fluid buildup.
CT Calcium Score: Measures the amount of calcium deposited on the valve.
Cardiac Catheterization: A thin tube (catheter) is passed through an artery to the heart to measure blood pressure and oxygen levels—this gives an accurate measurement of the pressure across the valve.
Dobutamine Stress Echo: Especially useful in cases with low blood flow (low-flow/low-gradient stenosis), this test helps determine how tight the valve truly is and how well the heart is functioning.
4. Cardiac MRI / CT Scan : These advanced imaging techniques provide precise information about the size of the aorta, the structure of the valve, and the amount of calcium present. They are especially helpful when the echocardiogram does not give complete information or when planning for surgery.
5. Role of Specialists : After diagnosis, a cardiologist evaluates the severity of the condition and any associated illnesses to create a treatment plan. In many cases, a full heart team — including a cardiac surgeon, interventional cardiologist, and other specialists — works together to determine the best option for you.
Aortic valve stenosis is not identified through a single test but through a combination of clinical evaluation and modern imaging techniques. Getting timely tests is the key to understanding the severity of the disease and starting the right treatment at the right time.
How many stages does this disease have?
Aortic valve stenosis is a gradually progressive disease. Doctors classify its severity into four main stages — A, B, C, and D. Each stage represents a different condition of the disease and guides the direction of treatment.
1. Stage A – At-risk stage: In this stage, the person does not yet have the disease, but the risk factors are present.
- Mild calcium buildup or thickening may be seen on the aortic valve, but it does not yet affect blood flow.
- The velocity of blood flow through the valve is less than 2 meters per second.
At this level, the most important things are: a healthy lifestyle, regular health check-ups, and controlling risk factors such as high blood pressure, cholesterol, and smoking.
2. Stage B – Progressive stage: In this stage, the disease has begun, but the person still has no symptoms.
- The valve becomes slightly stiff and narrow, causing mild to moderate obstruction to blood flow.
- Regular echocardiography is very important to monitor how quickly the narrowing is progressing.
Doctors usually advise lifestyle modifications and an annual or biennial echocardiogram.
3. Stage C – Severe but asymptomatic stage: In this stage, the narrowing of the valve becomes severe, but the person still does not experience symptoms. At this level, the disease is “silent,” yet it puts significant pressure on the heart.
This stage is divided into two subcategories:
- C1: The valve is severely narrow, but the heart’s pumping capacity (Ejection Fraction – EF) remains normal.
- C2: The valve is severely narrow and the EF falls below 50%, indicating that the heart's strength is beginning to decline.
Doctors usually recommend close monitoring (echocardiogram every 6–12 months), and in some cases, valve replacement may be advised to prevent further deterioration of heart function.
4. Stage D – Severe and symptomatic stage: This is the most dangerous stage of the disease, where symptoms appear clearly.
- The patient experiences shortness of breath, chest pain, dizziness, or fainting.
- At this stage, the valve is extremely narrow, and the heart must work very hard to pump blood.
This stage is further divided into three subcategories:
- D1 (High-gradient AS): Blood flow velocity across the valve is ≥4 m/s or the pressure gradient is ≥40 mmHg — indicating significant obstruction.
- D2 (Low-flow/Low-gradient AS with reduced EF): The heart's pumping strength has decreased, so the pressure appears lower even though the valve is very narrow.
- D3 (Low-flow/Low-gradient AS with normal EF): The pumping strength is normal but the stroke volume is low, causing reduced blood flow.
At this stage, immediate treatment is necessary — typically surgical or transcatheter valve replacement (SAVR/TAVR), which is considered a life-saving option.
What are the goals of treatment?
The main purpose of treating Aortic Valve Stenosis is not only to control the disease but also to keep the heart healthy and functioning well for a long time. Since this disease progresses slowly and affects the heart’s pumping ability, the treatment plan must be made thoughtfully and in a step-by-step manner. There are three main goals of treatment:
1. Reducing Symptoms :
The first goal of treatment is to reduce the symptoms of the disease and improve the patient’s quality of life. Doctors use certain medications to reduce the pressure on the heart and help maintain smooth blood flow.
When symptoms improve, patients are able to perform daily activities like walking, climbing stairs, or doing light exercise more comfortably. Although medicines cannot open the narrowed valve, they can provide relief and stability until valve replacement becomes necessary.
2. Preventing Damage to the Left Ventricle :
In aortic valve stenosis, the left side of the heart — known as the left ventricle — is most affected. When the valve narrows, the heart must use more force to pump blood. Over time, this continuous pressure can cause the walls of the left ventricle to thicken and the heart muscle to weaken. This can eventually lead to heart failure.
The second major aim of treatment is to:
- Reduce this extra pressure,
- Protect the strength of the heart muscle, and
- Address the problem before permanent damage occurs.
- 3. Timely Valve Replacement :
Valve replacement is the only definitive treatment for this disease—because medications cannot correct the narrowing. Therefore, the third and most important goal is to recognize the right time to replace the valve.
- Doing surgery too early may increase unnecessary risks.
- While delaying it too long may cause permanent damage to the heart.
This is why doctors determine the timing of surgery based on regular echocardiography, symptom monitoring, and other evaluations
What are the treatment options?
Treatment depends on the severity of your condition and the symptoms you experience. All patients require regular follow-up and monitoring.
1) Monitoring (if the disease is mild) ; In mild cases, only regular follow-up and echocardiographic monitoring are needed.
Control blood pressure, sugar, and cholesterol; stop smoking; and engage in regular light to moderate exercise (but avoid heavy exertion or sports in symptomatic aortic stenosis).
2) Medications:
- Rhythm/rate-controlling medicines (to keep the heartbeat regular).
- Blood thinners (Anticoagulants): to prevent blood clots, in specific situations.
- Antibiotics: for infection prevention, as advised by the doctor.
Important caution: In severe aortic stenosis, some vasodilators can cause a sudden drop in blood pressure — they should be used only under strict medical supervision.
3) Valve Replacement — the definitive treatment :
- Open-heart surgery (SAVR): A large incision is made, and the valve is replaced with a mechanical or bioprosthetic valve.
- Transcatheter Aortic Valve Replacement (TAVR): A new valve is inserted via a catheter through a small incision (usually through the femoral artery).
This is the actual “cure” for the disease — medicines do not widen the valve; they only help manage symptoms until valve replacement is needed.
Which treatment is right for you?
The choice of treatment is carefully made by a specialized heart-valve team—including a cardiologist, cardiac surgeon, and interventional specialist. They decide the best option after assessing your surgical risk, age, frailty, associated health conditions, the condition of your arteries and coronary vessels, and your personal preferences.
- If you have multi-vessel coronary artery disease, a combination of SAVR (surgical valve replacement) with CABG (bypass surgery) is often considered the most suitable approach.
- If you are at very high surgical risk or are not fit for open-heart surgery, then TAVR becomes the preferred treatment option.
How should you take care after a valve replacement (basic guidance)?
Proper care after aortic valve replacement is extremely important because it ensures the protection of the new valve, improves heart function, prevents complications, and helps make recovery safe and effective.
- Follow the doctor’s instructions regarding blood thinners/antiplatelet medicines (warfarin/aspirin/clopidogrel), including regular INR monitoring.
- Before any dental procedure, antibiotic prophylaxis for infective endocarditis may be advised in certain situations—keep written advice or instructions from your cardiologist with you for this purpose.
- Cardiac rehabilitation/regular walking, strict control of blood pressure and blood sugar, and complete avoidance of smoking.
What should be avoided? (Pitfalls)
Certain precautions are very important during the treatment and monitoring of aortic stenosis, because even small mistakes can lead to serious complications. The points below explain which situations and errors should be avoided so that treatment remains safe and effective.
- In symptomatic aortic stenosis, doing an exercise stress test is prohibited — it carries a risk of complications.
- In heart failure + severe aortic stenosis, giving vasodilators without monitoring can be dangerous.
- Many elderly patients have multiple comorbidities — a team-based approach is needed to clarify whether the symptoms are due to aortic stenosis or something else.
How should home care and lifestyle be?
In aortic valve stenosis, along with medicines and medical treatment, home care and a healthy lifestyle play a very important role. This not only helps control symptoms but also slows the progression of the disease and protects the heart. The following measures serve as a guide for patients and their families:
1. Diet:
- Heart-healthy diet: fresh vegetables and fruits, whole grains, low-fat dairy, pulses/lean protein.
- Low salt, low sugar, low saturated fat.
- Limit caffeine (it can affect heart rate/rhythm).
- Reduce canned/processed/fried foods.
2. Daily routine
- Exercise regularly — but decide with your doctor how much and what kind.
- In mild cases, only very intense exercise (like heavy weight lifting) may need to be avoided.
- As severity increases, additional restrictions on activity may be required.
3. Keep blood pressure, sugar, and cholesterol within target levels; take medicines regularly.
4. Maintain a healthy weight.
5. Limit alcohol:
- 0–1 drink/day for women, 0–2 drinks/day for men (1 drink = 355 mL beer, or 148 mL wine, or 44 mL hard liquor).
6. Avoid all forms of tobacco/nicotine completely (cigarettes, vaping, chewing tobacco, etc.).
7. If asymptomatic: Do 30 minutes of light–moderate exercise daily (as advised by your doctor).
8. If symptomatic: Avoid heavy exertion/running; discuss travel/work plans with your doctor.
9. Do not miss echocardiogram dates; if symptoms worsen, do not wait for the next appointment — seek medical help immediately.
10. Maintain good oral hygiene; consult your cardiologist before any major dental procedure.
11. Keep your echocardiogram reports and list of medicines with you; they are useful in an emergency.
When to seek immediate help?
In patients with aortic valve stenosis, certain symptoms can suddenly become severe and life-threatening. At such times, seeking medical help immediately is extremely important. Consider the signs listed below as an emergency and go to the hospital right away or call for assistance.
Any of the following symptoms should be treated as an emergency:
- Chest pain or tightness
- Difficulty breathing
- Feeling dizzy or about to faint
- Heartbeat becoming very fast or irregular
Call the emergency number immediately — 108/112.
Do not wait, and do not drive yourself to the hospital.
The right treatment is the key to life
Aortic valve stenosis is a heart condition that progresses slowly, but if not diagnosed and treated in time, it can become life-threatening. In this disease, the heart valve becomes narrow, which obstructs blood flow and forces the heart to work harder than normal.
Therefore, getting timely echocardiography, taking symptoms seriously, and undergoing valve replacement (SAVR or TAVR) at the right time are extremely important. These steps ensure both your quality of life and your safety.
If you experience symptoms such as shortness of breath, chest pain, dizziness, or fainting, do not ignore them — contact a cardiologist immediately. Early evaluation and treatment can prevent serious complications such as heart failure.
Lindman BR et al: Aortic valve disease. In: Zipes DP et al, eds: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Elsevier; 2019:1389-414
Nishimura RA et al: 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 135(25):e1159-95, 2017
Dr Prem Aggarwal, (MD Medicine, DNB Cardiology) is a Cardiologist by profession and also the Co-founder of Medical Dialogues. He is the Chairman of Sanjeevan Hospital in Central Delhi and also serving as the member of Delhi Medical Council

