- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
- Home
- Latest News
- Health Topics
- Health Tube
- MDTV
- Viral Sach (Fact Check)
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and Oral health fact check
- Diabetes and Metabolic Health fact check
- Diet and Nutrition Fact Check
- Eye Health Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Liver health fact check
- Medical education fact check
- Men's health fact check
- Neurology Fact Check
- Respiratory Fact Check
- Skin and Hair Care Fact Check
- Vaccine and Immunization fact check
- Women's health fact check
- Health FAQ
- Vaccines
- Web Stories
Stabbing chest pain, sharp discomfort or pounding heartbeat? It may be pericarditis — know the symptoms, tests and treatment?
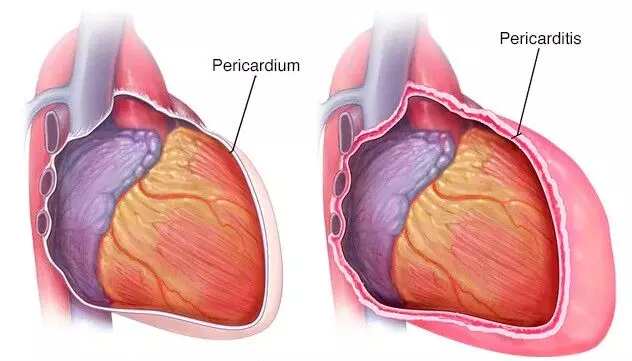
Our heart beats day and night — about 70 times per minute, which means more than one lakh times a day. To protect this delicate organ that works so hard, nature has created a special covering — the Pericardium. It is a thin, double-layered membrane that surrounds the heart like a pouch.
Inside this membrane is a small amount of fluid, called Pericardial fluid. This fluid reduces friction between the two layers of the membrane during each heartbeat, allowing the heart to function smoothly. It acts as the heart’s “protective shield,” safeguarding it from external shocks, infections, and excessive expansion.
What is Pericarditis?
Pericarditis is the inflammation of the thin membrane (pericardium) that surrounds the heart. Sometimes due to an infection, injury, or other causes, this membrane becomes inflamed.
When this happens, the two layers of the pericardium rub against each other and the fluid between them may increase, leading to symptoms such as sharp chest pain, difficulty breathing, and a sensation of rapid or forceful heartbeats.
This condition may be mild, but at times it can become serious. Therefore, understanding its symptoms and seeking timely medical advice is extremely important.
What are the types of Pericarditis?
Pericarditis can appear in several different forms, and understanding these types is important for correct diagnosis and treatment.
- Acute Pericarditis: Begins suddenly and usually resolves within a few days or weeks.
- Subacute Pericarditis: Develops gradually, with symptoms appearing over several days.
- Recurrent Pericarditis: Returns after an initial episode, typically after a symptom-free period of 4–6 weeks or longer.
- Chronic Pericarditis: When the inflammation lasts for more than 3 months or keeps recurring frequently.
- Constrictive Pericarditis: The layers of the pericardium become thickened and stiff, reducing the heart’s ability to expand and contract properly. This is rare but serious.
Most cases of pericarditis are acute and resolve on their own, but chronic and constrictive forms often require long-term treatment.
When should it be considered an emergency?
The situations below can be life-threatening — seek emergency care immediately:
● Signs of cardiac tamponade:
Rapid or difficult breathing, extreme weakness, near-fainting or fainting, drop in blood pressure, fast heartbeat, and muffled or faint heart sounds.
● Suspected purulent (pus-filled) pericarditis:
High fever, chills, and signs of sepsis — these cases may require urgent pericardiocentesis (removal of fluid from the pericardial sac).
Why is it important to recognize the symptoms?
The symptoms of pericarditis often resemble those of heart pain or even a heart attack, which makes it essential to understand and identify them correctly.
This condition may develop gradually or may appear suddenly with sharp chest pain. The signs and symptoms listed below act as warning signals from your body, helping you seek timely diagnosis and treatment.
🔸 Major Symptoms
• Sharp, stabbing chest pain that worsens while breathing, coughing, or lying down;
relief on sitting up or leaning forward is a characteristic feature.
• Pain spreading to the neck, shoulder, back, or trapezius muscles.
• Doctors may sometimes hear a pericardial friction rub — a scratchy, squeaking sound — during auscultation.
🔸 Other Symptoms
Along with the main symptoms, pericarditis can present with several additional signs, which are important to recognize for timely treatment:
● Dry cough
● Fast or irregular heartbeats (palpitations)
● Fever and body aches
● Fatigue and weakness
● Dizziness or fainting
● Shortness of breath, especially while lying down
● Occasional hiccups or changes in voice
Do not ignore these signs. Seek medical advice promptly if any of them appear.
What causes Pericarditis?
Pericarditis is not just a simple inflammation; it can be a sign of several hidden illnesses, infections, or problems in the body’s immune system. Sometimes it appears suddenly without any clear reason. Understanding the possible causes of pericarditis is very important for timely treatment and preventing complications.
1. Infectious Causes (Infections)
● Viral infections (most common): Such as Coxsackie virus, influenza, HIV, or adenovirus.
● Bacterial infections: Tuberculosis (TB) is a major cause; other bacteria include Staphylococcus and Streptococcus (pneumococcus).
● Fungal infections: Seen more often in people with a weakened immune system.
● Parasitic infections: Very rare (such as Echinococcus).
2. Non-Infectious Causes
● Autoimmune diseases: Conditions in which the body’s immune system attacks its own tissues — such as lupus, rheumatoid arthritis, vasculitis, etc.
● Heart attack (Myocardial Infarction): Inflammation may develop a few days or weeks after a heart attack.
● Cancer: Spread of cancers such as lung cancer, breast cancer, or lymphoma to the pericardium.
● Hypothyroidism and Kidney failure (Uremia).
● Radiation therapy: Damage to the pericardium after radiation treatment for cancer.
● Medications: Some heart medicines, anti-seizure drugs, and blood thinners (such as hydralazine, phenytoin, warfarin).
● Chest injury or after open-heart surgery.
Who is at Higher Risk of Developing Pericarditis?
Certain individuals are more vulnerable to Pericarditis due to underlying medical or lifestyle-related factors. If you fall into any of the categories below, your chances of developing this condition may be higher than average:
● Men — Studies show that men have nearly twice the risk compared to women.
● Adults aged 20–50 years — Pericarditis is most commonly seen in this age group.
● Recent viral infection — A cold, flu, or other viral illness in the past few weeks can trigger inflammation of the pericardium.
● Previous history of pericarditis — Once you’ve had pericarditis, the likelihood of it returning (recurrence) increases significantly.
● Weakened immune system — People with reduced immunity are at higher risk, including those with:
- Diabetes
- Cancer or undergoing chemotherapy/radiation
- HIV infection
- Long-term steroid use
- Patients on immunosuppressive drugs (such as after organ transplant or for autoimmune diseases)
Why should Pericarditis not be taken lightly?
Although Pericarditis often improves on its own in many cases, it can sometimes become serious and directly affect the functioning of the heart.
If the inflammation is not controlled in time, or if the underlying cause is severe, several complications may develop—some of which can be life-threatening. This is why recognizing its symptoms early and seeking appropriate medical care is extremely important.
1. Pericardial Effusion (Excess fluid between the pericardial layers):
This can increase pressure around the heart and lead to symptoms such as shortness of breath and discomfort.
2. Cardiac Tamponade:
When fluid accumulates to such an extent that it compresses the heart, it becomes a life-threatening condition. It may cause a drop in blood pressure, fainting, and severe breathing difficulty. This is a medical emergency.
3. Constrictive Pericarditis:
If inflammation persists for a long time, the pericardial layers can become thick and stiff. This reduces the heart’s ability to expand and contract properly, causing ongoing symptoms such as swelling in the legs, breathlessness, and fatigue.
4. Recurrence (Recurrent Pericarditis):
In many patients, pericarditis can return repeatedly. Even with proper treatment, the condition may recur after months or years, especially if the cause is autoimmune or viral.
Recognizing these complications early and getting appropriate treatment can help prevent serious outcomes. Therefore, never ignore Pericarditis — vigilance is the best protection for your heart.
How Do Doctors Diagnose Pericarditis?
Diagnosing Pericarditis requires careful evaluation because its symptoms often resemble those of a heart attack or other serious heart conditions. Doctors rely on a combination of medical history, physical examination, and specialized tests to confirm the diagnosis and understand the severity of the condition.
1. Physical Examination
- Doctors listen to the heart using a stethoscope.
- A distinctive sound called a “pericardial friction rub” may be heard — a scratchy, squeaking, or grating noise caused by the inflamed pericardial layers rubbing against each other.
This finding is considered one of the hallmark signs of pericarditis.
2. Diagnostic Tests
As Pericarditis can mimic other heart illnesses, several tests are used to confirm the diagnosis and rule out dangerous conditions:
• ECG (Electrocardiogram) : An ECG is often the first test performed. It can show typical electrical changes, such as:
- ST-segment elevation
- PR-segment depression
These findings help distinguish pericarditis from a heart attack.
• Echocardiography (Heart Ultrasound): This is one of the most important tests. It helps detect:
- Fluid buildup around the heart (pericardial effusion)
- educed heart movement
- Early signs of cardiac tamponade (a medical emergency)
• Chest X-ray: A simple chest X-ray can reveal:
- An enlarged-looking heart, which may indicate a large pericardial effusion
- Associated lung or chest abnormalities
• CT Scan or MRI : These advanced imaging tests are used when the diagnosis is unclear or complications are suspected. They help identify:
- Pericardial inflammation
- Thickening or scarring
- Constrictive pericarditis
• Blood Tests : Laboratory tests help identify inflammation, infection, or associated conditions:
- CBC (Complete Blood Count)
- ESR/CRP — markers of inflammation
- Troponin — detects heart muscle injury
- Thyroid function test
- Kidney function test
- Blood cultures — especially if bacterial infection or pus is suspected
• Pericardial Fluid Analysis : If there is fluid around the heart, a small sample may be extracted to check for:
- Bacteria
- Cancer cells
- Tuberculosis
- Signs of infection or inflammation
This test helps pinpoint the exact cause of pericarditis.
• Biopsy or Cardiac Catheterization : These are rarely needed but may be recommended when:
- Constrictive pericarditis is suspected
- Initial tests are inconclusive
- A more detailed assessment of heart pressures is required
Pericarditis is diagnosed using a combination of clinical clues and modern tests. Early and accurate diagnosis is essential to start proper treatment and prevent serious complications like cardiac tamponade or constrictive pericarditis.
What Are the Goals of Treating Pericarditis?
The primary goals of treating pericarditis are to relieve pain, reduce inflammation, prevent the condition from worsening, and avoid long-term complications such as cardiac tamponade or constrictive pericarditis. Treatment depends on the severity of symptoms and the underlying cause.
1. Lifestyle Measures and Rest : Rest plays a crucial role in recovery because physical exertion can worsen inflammation.
- Limit physical activity until pain, breathing difficulty, and inflammation fully subside.
- Athletes should avoid competitive sports for at least three months, as intense exercise can trigger recurrence.
- Maintain a heart-healthy lifestyle — adequate sleep, stress reduction, low-salt diet, and plenty of fruits and vegetables.
- Avoid strenuous activities, long walks, running, or workouts during recovery.
2. Medications: Different medicines are used depending on the cause and severity of pericarditis:
• NSAIDs (Ibuprofen, Aspirin) : These are the first-line treatment. They help reduce chest pain and decrease inflammation in the pericardium.
• Colchicine : A key medication for pericarditis helps settle inflammation more quickly and significantly reduces the risk of the condition returning. It is often used together with NSAIDs.
• Corticosteroids (e.g., Prednisolone): Used when NSAIDs do not work or when the cause is autoimmune. These must be tapered slowly to avoid recurrence.
• Antibiotics or Antivirals : Given when a confirmed infection—bacterial, viral, or tuberculous—is responsible for causing pericarditis.
• IL-1 Blockers (Rilonacept, Anakinra) : These are advanced treatments used mainly in recurrent cases where standard therapy don't respond. They require special approval and specialist supervision.
3. Procedures and Surgical Options
• Pericardiocentesis : A procedure in which a needle and catheter are used to drain excess fluid around the heart. It is required when the fluid buildup causes pressure on the heart (cardiac tamponade) or when infection is suspected.
• Pericardiectomy : A major surgery in which part or all of the pericardium is removed.
This is reserved for Constrictive pericarditis or severe & recurrent cases that do not respond to any medication
Who Needs Hospitalization?
Most patients with Pericarditis can be treated at home with medication and rest. However, certain situations indicate that hospital admission is absolutely necessary, as they suggest a severe form of the disease, possible complications, or potential danger. Delaying care under such circumstances can lead to serious consequences.
Below are the key situations in which a patient must be admitted to the hospital immediately for proper evaluation and treatment:
1. High fever (above 100.4°F / 38°C) : A high-grade fever may signal a serious infection such as tuberculosis or bacterial pericarditis, which cannot be safely treated outside the hospital.
2. Subacute onset : If the illness develops gradually over several days, it may indicate more complex causes—such as TB or autoimmune diseases—requiring detailed evaluation.
3. Large pericardial effusion : When an excessive amount of fluid collects around the heart, it can increase pressure on the heart. This condition may worsen quickly and needs continuous monitoring in a hospital setting.
4. Suspected cardiac tamponade : If fluid builds up to a point where it compresses the heart, it becomes a life-threatening emergency. Symptoms include:
- Shortness of breath
- Low blood pressure
- Fainting
- Extreme weakness
This is a medical emergency requiring immediate hospital care.
5. No improvement after 7 days of NSAIDs : If there is no response to standard treatment, it may indicate a deeper or more serious underlying cause (such as TB, autoimmune disease, or drug-related inflammation).
6. Weakened immune system (Immunosuppression) : Patients with Cancer, HIV, taking steroids or on immunosuppressive medications; have a higher risk of rapid progression of infection and must be treated in a hospital setting.
7. Chest injury or recent surgery : Pericarditis developing after trauma or open-heart surgery can take a severe form and requires careful monitoring.
8. Patients on anticoagulant medications : Blood thinners increase the risk of bleeding into the pericardial sac (hemopericardium), which is potentially life-threatening and requires hospital-based monitoring.
9. Elevated troponin levels (suggestive of myocarditis) : When troponin is elevated, it indicates that the heart muscle itself is involved (myopericarditis). Such patients need close monitoring and specialized treatment in a hospital.
When is ICU Care Needed?
Some severe forms of pericarditis can cause the patient’s condition to deteriorate rapidly, requiring urgent expert care. When the heart is under pressure or blood pressure becomes unstable, treatment in a regular ward is not safe.
In such situations, the patient must be admitted to the ICU for continuous monitoring and immediate intervention, especially in cases of suspected or confirmed cardiac tamponade or hemodynamic instability.
Pericarditis can be mild or serious—everything depends on how quickly the symptoms are recognized and treated. If you or someone you know has any of the warning signs listed above, hospital admission can be life-saving. Never delay or ignore symptoms when it comes to heart health.
Follow-up and Monitoring
Treatment for pericarditis does not end with taking medications — it requires proper follow-up, regular testing, and careful adjustment of medicines. Even after the symptoms improve, it is essential to assess the heart’s recovery to detect complications, recurrence, or the development of constrictive pericarditis at an early stage.
● CRP, ECG, and Echocardiography are used to confirm improvement.
● In post–cardiac-injury syndrome, an echocardiogram at 6–12 months is recommended to check for progression toward constrictive pericarditis.
● Medications must be tapered gradually and never stopped abruptly, as sudden discontinuation increases the risk of recurrence.
What to Expect Going Forward? (Prognosis)
The outlook for pericarditis varies widely and depends mainly on two factors; the underlying cause and how early the condition is diagnosed and treated. With timely care, most patients recover fully and lead completely normal lives.
- In most viral or idiopathic (unknown cause) cases, the illness resolves on its own within a few weeks, and the long-term outlook is generally very good.
- If colchicine is not taken, the condition may recur in about 15–30% of patients. Taking colchicine cuts the risk of recurrence by nearly half.
- The severity and future outcomes depend on the cause:
* Viral or idiopathic pericarditis rarely leads to major long-term problems.
* Tuberculous or bacterial (purulent) pericarditis tends to be more serious and carries a higher risk of complications.
- If purulent pericarditis is not treated promptly, it can become life-threatening.
However, with timely fluid drainage and appropriate antibiotics, the results improve significantly.
What precautions should be taken at home?
Most of the treatment for pericarditis can be safely managed at home, but only if you strictly follow your doctor’s instructions.
Proper home care can speed up recovery, reduce pain and inflammation, and significantly lower the risk of the condition returning (recurrence). The precautions below make your healing process safer and more effective:
● Never ignore sharp or persistent chest pain.
● Follow your doctor’s advice carefully — ensure adequate rest, take your medications on time, and complete all recommended follow-up tests.
● Avoid alcohol, smoking, and the random use of over-the-counter painkillers.
● People at higher risk — such as those prone to tuberculosis, or those with cancer, autoimmune diseases, or on dialysis — should seek medical attention immediately if they develop new chest pain or fever, even if the symptoms seem mild.
Timely Recognition and Proper Care Are Your Best Protection
Pericarditis is usually a manageable and treatable condition—provided its early warning signs are recognized on time and the right tests and treatment are carried out promptly.
However, some complicated forms—such as cardiac tamponade or purulent pericarditis—can become life-threatening very quickly and require immediate hospital care.
Therefore, if your chest pain eases when sitting up or leaning forward, or if you experience persistent fever, shortness of breath, rapid heartbeat, dizziness, or a fainting sensation, do not make the mistake of dismissing these symptoms as minor.
Prompt evaluation and consultation with a specialist are the safest ways to prevent serious complications.
Doctor NS et al: Acute pericarditis. Prog Cardiovasc Dis. 59(4):349-59, 2017
Kloos JA: Characteristics, complications, and treatment of acute pericarditis. Crit Care Nurs Clin North Am. 27(4):483-97, 2015
USFDA. FDA Approves First Treatment for Disease That Causes Recurrent Inflammation in Sac Surrounding Heart. USFDA website. Updated March 18, 2021. Accessed October 10, 2024. https://www.fda.gov/drugs/drug-safety-and-availability/fda-approves-first-treatment-disease-causes-recurrent-inflammation-sac-surrounding-heart
Imazio M et al: Recurrent pericarditis. Rev Med Interne. 38(5):307-11, 2017
Dr Prem Aggarwal, (MD Medicine, DNB Cardiology) is a Cardiologist by profession and also the Co-founder of Medical Dialogues. He is the Chairman of Sanjeevan Hospital in Central Delhi and also serving as the member of Delhi Medical Council

