Multiple Sclerosis Care in India Needs Urgent Overhaul, Say Experts at National Conference
New Delhi: The Multiple Sclerosis Society of India (MSSI) – Delhi Chapter, in collaboration with G. B. Pant Institute of Postgraduate Medical Education and Research and the Association of Neurological Science and Research, hosted a national conference titled "Navigating MS: Landscape, Gaps and Opportunities" at the India Habitat Centre.
The event brought together leading neurologists, public health experts, policymakers, patient advocacy groups, and individuals living with Multiple Sclerosis (MS) to discuss the multi-dimensional challenges of managing MS in India.
With over 1.5 lakh people estimated to be living with MS in India, most between the ages of 20 and 40, the conference focused on bridging critical gaps in early diagnosis, access to treatment, disability rights, mental health, and social inclusion. It also explored the integration of precision medicine and novel therapies into India’s healthcare delivery system.
Inaugurating the event, Ms. Bipasha Gupta, Honorary Chairperson of MSSI – Delhi Chapter, stressed the importance of patient-centric action and collective responsibility.
"Multiple Sclerosis is often called an invisible illness, but for those living with it, the challenges are constant and deeply personal—ranging from unpredictable symptoms to emotional, social, and financial burdens. This year we are celebrating the 40th anniversary of MSSI, where we stand not only as a support system but also as a driving force for change. This platform allows us to amplify patient voices, share real experiences, and push for timely diagnosis, evidence-based care, and stronger public health support. Together, we are working towards a future where no one faces MS alone—and every patient receives the care, dignity, and opportunities they deserve," she said.
Delivering a strong policy perspective, Dr. Ashish Duggal from RML Hospital emphasized the urgent need for systemic reforms.
"The current landscape of MS care in India is fragmented. While we have made strides in treatment options, the lack of a centralized policy framework leaves thousands without timely access to life-changing therapies. MS must be integrated into the National Health Mission and recognized under the Rare Disease Policy and Ayushman Bharat to ensure equitable care and access to drugs. Additionally, insurance providers must update their coverage to include advanced Disease-Modifying Therapies (DMTs), which are proven to delay disability progression," he said.
Dr. Duggal also highlighted the limitations of current disability certification frameworks.
"Another critical gap is disability certification—many MS patients suffer from invisible symptoms like fatigue, cognitive fog, and neuropathic pain, which are not adequately recognized under current disability laws. We need revised guidelines that account for these challenges to ensure patients receive the financial and social support they deserve," he added.
Dr. Rajesh Iyer of Poorna Neuro Clinic, Bengaluru, pointed out the risk of misdiagnosis and the need for improved diagnostic protocols.
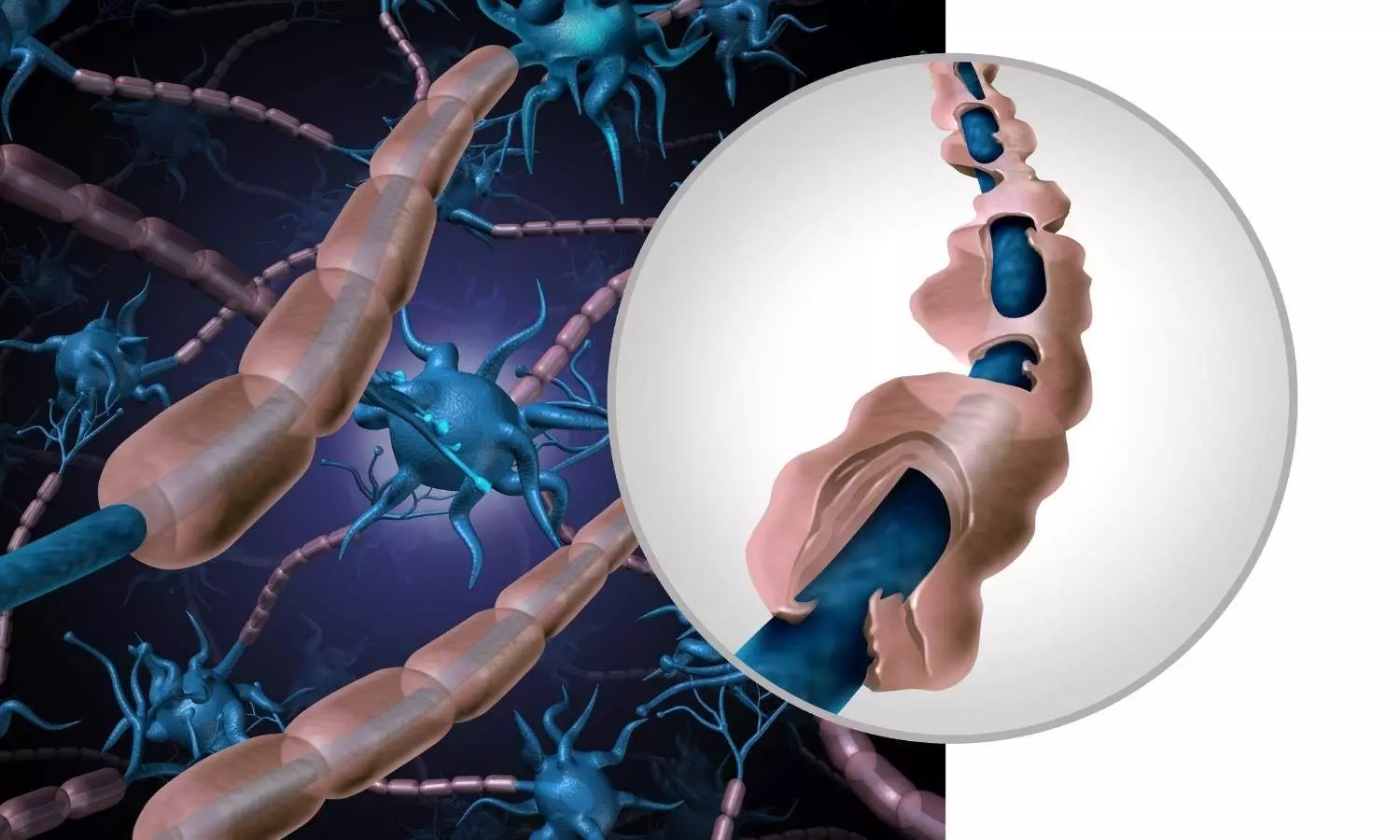
"MS can be misdiagnosed with other neurological conditions like neuromyelitis optica, MOGAD, lupus, or even vitamin deficiencies. Early and accurate diagnosis is crucial because initiation of appropriate early treatment can prevent future disabilities. It is important to maintain NEDA (No evidence of disease activity). Relapses and PIRA cause lots of neurons leading to accumulating disability over time. Advanced imaging techniques (MRI) with special protocols for MS and demyelinating disorders and other blood/CSF biomarkers can improve diagnostic accuracy. Additionally, raising awareness among general physicians and public about initial symptoms of MS—such as optic neuritis, unexplained numbness, or balance issues—can help reduce diagnostic delays, especially in smaller towns where neurologists are scarce."
Dr. M. Netravathi from NIMHANS, Bengaluru, spoke about the emergence of precision medicine in MS treatment.
"The era of ‘one-size-fits-all’ MS treatment is ending. Today, we can tailor therapies based on a patient’s genetic predisposition, disease subtype (relapsing-remitting vs. progressive), and even lifestyle factors. For instance, patients with aggressive MS may benefit from early high-efficacy therapies (HETs), while others might respond better to oral DMTs. The future lies in precision medicine—combining clinical data, imaging, and molecular profiling to optimize outcomes while minimizing side effects."
Raising the issue of societal challenges, Dr. MV Padma, Chairperson - Neurology, Paras Health, emphasized the stigma faced by MS patients.
"MS patients don’t just battle physical symptoms—they fight misunderstanding, workplace discrimination, and social isolation. Many are told, ‘You look fine, how can you be sick?’ because their disability is invisible. This leads to depression, job loss, and even marital strain. We need awareness campaigns and workplace protections to empower patients."
Speaking on the mental health burden, Dr. Manjari Tripathi, HOD - Neurology at AIIMS, highlighted a neglected but vital area of care.
"Nearly 50% of MS patients experience depression or anxiety, yet mental health remains a neglected aspect of care. The disease itself causes neuroinflammation that affects mood-regulating brain regions, while the stress of living with a chronic condition exacerbates psychological distress. We must integrate psychologists and psychiatrists into MS care teams. Cognitive behavioral therapy (CBT), mindfulness, and peer counseling should be standard alongside medication. Ignoring mental health undermines physical treatment and may be an important medication default."
The conference concluded with an urgent call for national standard-of-care guidelines, improved insurance frameworks, timely disability assessments, and collaborative research to elevate the quality of life for individuals living with MS across India.


