Uterine Fibroids: Insights into Causes, Symptoms, and Cutting-Edge Treatments - Dr Naveen Chandrashekhar
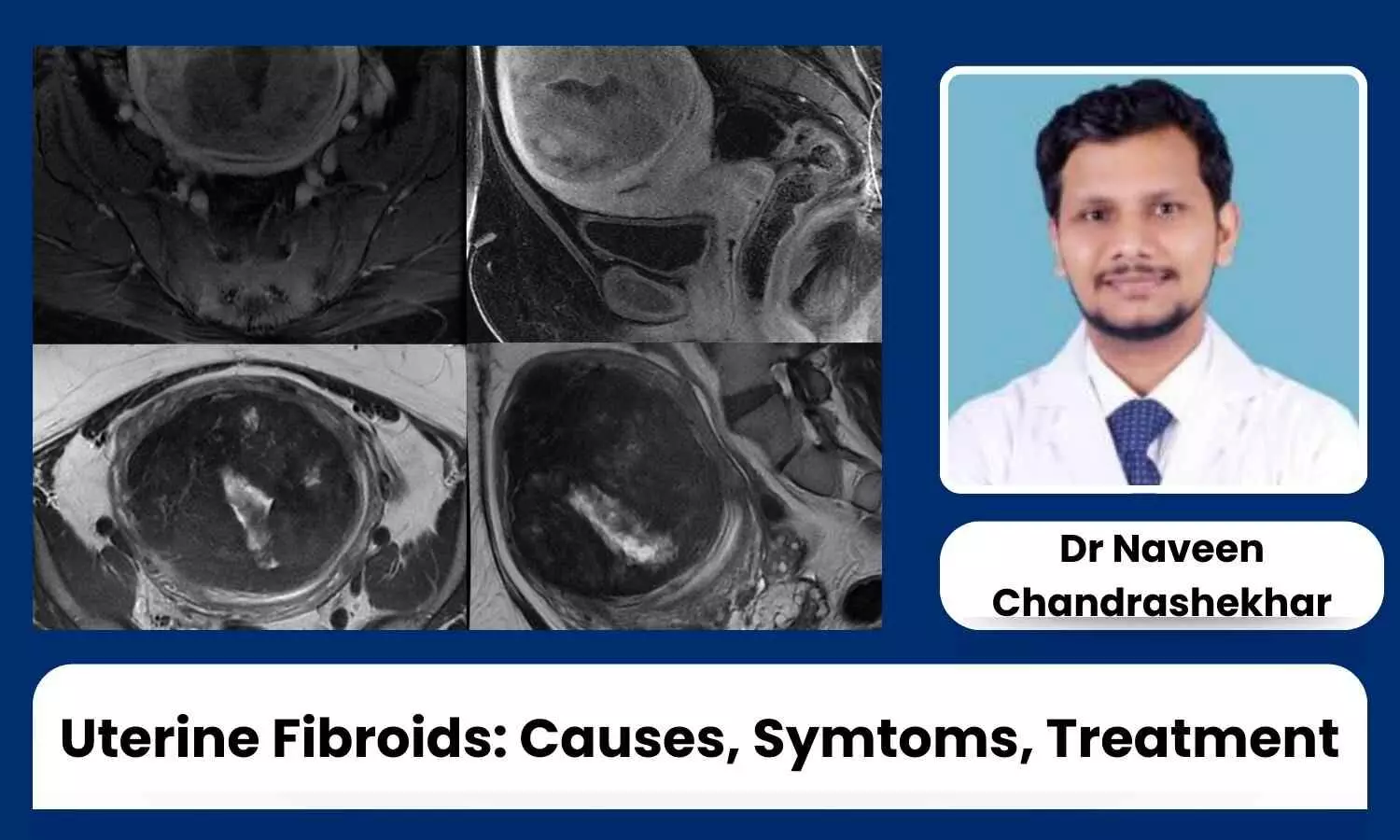
Uterine fibroids, also known as leiomyomas or myomas, are non-cancerous benign growths that develop in the muscular wall of the uterus. They are quite common, with around 20-80% of women developing fibroids by the age of 50. There are three types: intramural, submucosal, and subserosal.
Causes
The exact cause of uterine fibroids is not fully understood, but several factors may contribute to their development, including hormonal and genetic factors. Other risk factors include:
- Early menarche, late menopause
- Early childbirth
- Obesity, overweight
- High consumption of red meat, dairy, and chocolate products
- Higher prevalence in Asian populations compared to American populations
- Vitamin D deficiency
Symptoms
Symptoms of fibroids can vary but often include:
- Heavy menstrual bleeding (menorrhagia)
- Prolonged menstrual periods
- Pelvic pain or pressure
- Pain during intercourse
- Frequent urination or difficulty emptying the bladder
- Constipation or difficulty with bowel movements
- Backache or leg pains
- Enlargement of the lower abdomen or a feeling of fullness
Fibroids and Infertility
Uterine fibroids can potentially impact fertility, although the extent to which they affect fertility varies greatly among women. They can cause:
- Distortion of the uterine cavity
- Blockage of fallopian tubes
- Disruption of blood flow
- Alteration of uterine contractions
Medical Treatment for Fibroids
Medical treatments for fibroids include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Birth control pills
- Progesterone-releasing intrauterine device
- Gonadotropin-releasing hormone (GnRH) agonists
- Selective estrogen receptor modulators (SERMs)
- Tranexamic acid
- Iron supplements
Surgical Treatment for Fibroids
Surgical options include:
- Myomectomy (abdominal, laparoscopic, or hysteroscopic)
- Hysterectomy (abdominal or vaginal)
Minimally Invasive Advanced Non-Surgical Treatments for Fibroids
Advanced non-surgical treatments for fibroids include
1. Uterine Fibroid Embolization (UFE): UFE is a minimally invasive procedure in which tiny particles are injected into the blood vessels that supply the fibroids, cutting off their blood supply and causing them to shrink. This procedure is typically performed by an interventional radiologist and does not require surgical incisions.
2. Magnetic Resonance-Guided Focused Ultrasound Surgery (MRgFUS): MRgFUS uses high-intensity focused ultrasound waves to heat and destroy fibroid tissue while monitoring the process in real-time using MRI imaging. This noninvasive procedure is performed without incisions and allows for precise targeting of fibroids.
3. Radiofrequency Ablation (RFA): RFA uses heat energy delivered via a needle-like probe to destroy fibroid tissue. This minimally invasive procedure is typically performed under local anesthesia and ultrasound guidance and results in the shrinkage of fibroids.
4. High-Intensity Focused Ultrasound (HIFU): HIFU uses focused ultrasound waves to heat and destroy fibroid tissue. This noninvasive procedure is performed externally through the skin, without the need for incisions, and allows for precise targeting of fibroids.
These advanced non-surgical treatments offer alternatives to traditional surgical interventions for fibroids and can provide effective symptom relief with shorter recovery times and fewer complications. However, not all patients are suitable candidates for these procedures.
The choice of treatment depends on factors such as the size, number, and location of fibroids, as well as the patient's medical history and preferences. It’s essential for individuals with fibroids to consult with their healthcare provider to discuss the most appropriate treatment options for their specific situation.
IR vs. Traditional Surgical Techniques
Interventional radiology (IR) differs from traditional surgical techniques in several ways:
- Invasiveness: IR procedures are minimally invasive, involving small incisions or entry points, unlike traditional surgery, which often requires larger incisions.
- Imaging Guidance: IR procedures use imaging techniques (X-ray, ultrasound, CT scan, or MRI) to guide instruments and monitor the procedure in real-time, allowing for precise targeting.
- Anaesthesia: Many IR procedures can be performed under local anaesthesia or conscious sedation, reducing the need for general anaesthesia.
- Recovery Time: IR procedures generally have shorter recovery times, less pain, reduced scarring, and quicker return to normal activities compared to traditional surgery.
- Hospital Stay: IR procedures are often outpatient or require short hospital stays, whereas traditional surgeries may need longer hospitalizations.
- Risk of Complications: IR procedures usually have a lower risk of complications such as infection, bleeding, and postoperative pain.
What to Expect Before, During, and After UFE
Before the Procedure:
- Consultation: Discuss symptoms, medical history, and treatment options with an interventional radiologist.
- Pre-procedure Tests: Imaging tests (ultrasound, MRI, or CT scan) to assess fibroids.
- Pre-procedure Instructions: Instructions on fasting, medications to avoid, and other preparations.
During the Procedure:
- Anaesthesia: Local anaesthesia and conscious sedation.
- Catheter Insertion: Small incision in the groin, catheter insertion into the artery, advanced to the uterine arteries using fluoroscopy.
- Embolization: Tiny particles injected to block blood flow to fibroids, causing them to shrink.
- Monitoring: Continuous imaging to ensure accurate placement of embolic material.
After the Procedure:
- Recovery Room: Monitoring for immediate complications.
- Pain Management: Medications for cramping, pelvic pain, or discomfort.
- Hospital Stay: Usually a same-day procedure; most patients go home within a few hours.
- Recovery at Home: Post-procedure care instructions, including rest, activity restrictions, and medications.
- Follow-up: Follow-up appointments to monitor progress, assess symptom relief, and address concerns.
After UFE, expect a gradual improvement in symptoms such as heavy menstrual bleeding, pelvic pain, and pressure over the following weeks to months as the fibroids shrink. It’s essential to follow your healthcare provider’s instructions and attend all scheduled follow-up appointments to ensure optimal recovery and long-term outcomes.


